Lack of support and supplies raising alarm

Jay* is afraid to get out of their car. They are afraid of contracting COVID 19 and bringing it home to their family or ending up in the hospital or worse. The fact that they are double vaccinated against the virus doesn’t make a dent in their anxiety. They spoke to the Martlet on the condition of anonymity for fear of reprisal.
Jay is an experienced outreach worker in Victoria. Their days off are few and far between, and their anxiety attacks are becoming more and more frequent.
Despite the work done by BC Housing and organizations such as Our Place Society, many members of Victoria’s unhoused still don’t have access to proper supplies such as housing, food, or mental health supports.
With the fourth wave of the pandemic ripping its way through Victoria’s unhoused population, outreach workers like Jay are scared for the safety of their clients, their colleagues, and themselves.
“Assume everyone is infected”
Jay works with Sam*, another outreach worker who also wished to remain anonymous due to fears of reprisal. Sam told the Martlet that the situation is exacerbated by the lack of support available to those contracting COVID-19 in temporary and supportive housing environments.
Jay and Sam say that Island Health has given them next to no support and that their supplies of personal protective equipment (PPE) are dwindling. They say clients are leaving their buildings to venture for food and supplies, putting others at risk of infection. Capital Daily also reported that the unhoused have had no access to isolation beds.
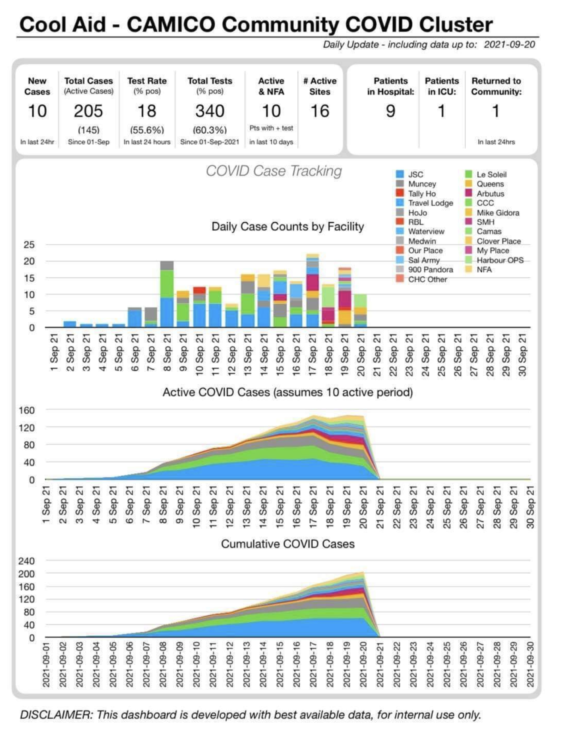
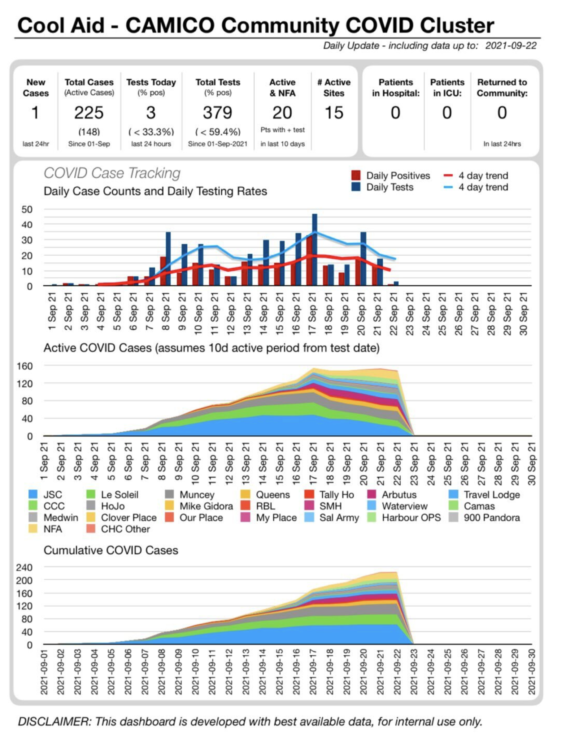
In early September, public health officials began noticing an uptick in infections amongst the province’s unhoused population, with the greatest surge occurring in Victoria. This was a surprise as, until that point, the local unhoused population had been largely spared from the COVID-19 pandemic.
The uptick came as the Delta variant of COVID-19 seeped into B.C. At that point, the data did not meet the criteria of an outbreak and public health officials were not concerned about the increase impacting the wider population. Outreach workers say that over Labour Day weekend what had been a trickle of cases quickly turned into a flood.
B.C. health officials announced 2 425 new cases over the Labour Day long weekend, up nearly 36 per cent from the week before.
Since then, cases have risen. A leaked Island Health internal report published first by Capital Daily put the number of cases amongst the unhoused at roughly 225 over the first three weeks of September. Island Health’s Dr. Richard Stanwick said in a press conference on Oct. 1 that the number is now around 300. Jay and Sam say this number is likely much higher.
“A lot of people aren’t getting tested,” Jay said.
Sam added that while they were initially able to get people tested with the help of Island Health, the system has become backlogged. They said that the wait to get tested is on average three days, and even longer for the unhoused as they don’t have the same access to transportation and communication services.
In an emailed statement to the Martlet, Island Health said that they have experienced a surge in calls for testing so people can expect longer than normal call-back times. Testing is being done on location, as needed.
Additionally, as much as 70 per cent of the unhoused remain unvaccinated due to concerns and conspiracy theories that are, at their root, a reflection of their mistrust of a health system that has failed to properly treat them in the past.
“It’s just really unfortunate,” said Sam. “Misinformation has been allowed to become a mainstream school of thought.”
Part of what is causing such anxiety for Jay and other outreach workers is the uncertainty of it all. They say that at the moment they have to assume that all of their clients are COVID-19 positive.
“That’s the reality of our jobs,” they said. “[But] how long is it going to take before we find bodies on the street dead from COVID?”
Lack of support
On top of dealing with the outbreaks, Jay and Sam say they are not being supplied with adequate PPE and have received very few messages from Island Health on how to conduct their outreach safely or help their clients isolate themselves if experiencing symptoms.
In their statement, Island Health said that outreach organizations are responsible for their own PPE and Island Health does not enforce isolation for anyone diagnosed with COVID-19.
In response to a lack of isolation spaces in Victoria, the Province, along with Island Health and the City of Victoria, announced last Friday that they would be developing 50 new spaces for isolation in Greater Victoria.
Of the new spaces, 30 will be in existing shelters, while the other 20 will be developed at a brand new site exclusively for isolation. All 50 units are expected to be ready by November.
B.C. Attorney General and Minister Responsible for Housing David Eby said that as of Thursday, isolation spaces had been found for all those who have tested positive. He says that there may be challenges, however, if cases continue to rise.
“There’s hardly any give left in the system,” he said. “This work is literally bed by bed and person by person.” In regards to keeping members of the unhoused in temporary facilities safe, organizations like Our Place are adhering to safety measures developed in concert with Island Health over the last 18 months of the pandemic.
“At every site, we have proper PPE for staff and residents,” said Our Place Society’s Director of Housing & Shelter Leah Young in an interview with the Martlet. “We have plans in place; if someone comes down with COVID, that includes meal delivery to their room and trying to support folks in isolation if they are positive.”
Jay and Sam say that they heard distancing measures aren’t being carried out at certain sites thus leading people to leave their rooms for food and other essentials. They say this is a result of a lack of staff who are struggling to meet the daily needs of their clients.
In an emailed statement to the Martlet, Our Place Director of Communications Grant McKenzie said that while Our Place is struggling with staff shortages like many other businesses, it has more than enough PPE to outfit staff.
“Our Housing Managers make sure all staff are provided personal PPE packs (shields, goggles, masks, gowns) as a part of their work tools,” he said. “Funnily enough, there were boxes of the stuff outside my office the other day as it was being sorted to top up the stock at all the housing sites.”
McKenzie also said that while they can remind residents to follow health mandates, they can’t force residents to wear masks or physical distance as the housing sites aren’t locked-down facilities.
“Just as we couldn’t enforce what you do in your own home, we can’t enforce what residents do in theirs,” said McKenzie. “Fortunately, the majority of residents who have tested positive have been self-isolating and taking proper measures as they simply don’t want to spread it to their fellow residents.”
According to Sam, the same goes for outreach workers who are facing staffing shortages with many quitting or taking time off due to anxiety. They say that because supportive housing and outreach are low-barrier services, they can’t enforce a need for clients to be vaccinated or to wear masks.
“If they come in, we say, ‘Would you like to put on a mask?’ that’s all you can do,” she said. “If they don’t, there’s no point in asking them five times because you’re going to be creating resentment, and you’re going to be creating a potential crisis, depending on the mood or how that person is doing.”
At the end of the day, Jay and Sam want to see the province and service providers step up and do their jobs in a way that protects those working on the front lines.
“We’re all understaffed,” said Sam. “We’re all running bare bones.”
*Jay and Sam spoke to the Martlet on the condition of anonymity for fear of reprisal. Their names have been changed for the article.







