History shows the significant changes prompted by past pandemics
It’s difficult to imagine what tomorrow will bring, much less what the world will look like when COVID-19 is eventually under control. But sometimes, the mind wanders. What lessons could the world learn from this pandemic, if any? Will we fix the problems highlighted by COVID-19, or just return to the previous status-quo?
It’s interesting to look back at previous pandemics, to see what the world learned from those experiences.
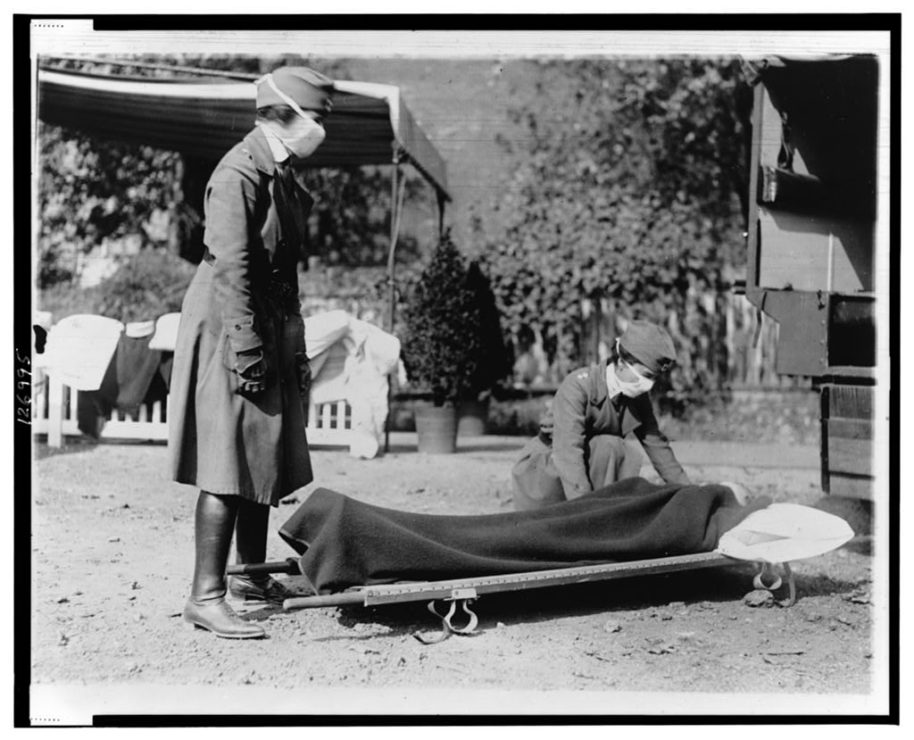
Before COVID-19, the most recent major pandemics were the Spanish Flu and HIV/AIDS. The Spanish Flu occurred in a very different environment: in 1918, there was no real structure to healthcare, which allowed for the illness to spread rapidly across the globe. There was no Ministry of Health, just doctors working for themselves or religious organizations. Unfortunately, it was commonly believed that sickness was eugenic in nature — meaning if you got sick, it was your fault and you deserved to get sick. When the first wave of Spanish Flu hit, people assumed that it was caused by bacteria. By the time quarantines and the shutdown of public places were implemented, it was too late. The systems in place couldn’t effectively treat people quickly, and get information out until the second wave of Spanish Flu swept across the world. Healthcare needed to become centralized in order to tackle something both on a local and universal level.
After HIV/AIDS, the largest changes to healthcare centered around the testing and screening of blood. It also prompted less frequent use of blood transfusions. Before HIV/AIDS, blood transfusions were more common. Nowadays, you have to lose a lot of blood to receive a transfusion, and now measures exist to save and/or retrieve a person’s own blood during surgery. After and during the Krever Inquiry, the investigation of how and why contaminated blood was still being used during the HIV/AIDS crisis and the active refusal to take steps to help Canadians in order to save money, the Canadian Blood Services was established for further protection of the public, as well as a tighter screening process for blood. Another notable change in the aftermath of AIDS was an increased use of gloves, masks, and gowns. They had to be introduced for universal protection during the pandemic, and their use was later scaled back for standard protection.
As for the future of the current pandemic, it’s difficult to say what it will look like. There may be an increased number of ventilators available, but it’s important to remember that this is an emergency situation. Hoarding supplies that you might not need later down the line — especially technology that might become outdated — isn’t a smart move.
For B.C, at least, there’s been a move towards a more centralized healthcare workforce when it comes to healthcare-aids, where workers at long-term care facilities work at one location full-time instead of multiple places part-time. This was done to protect vulnerable residents, as decreasing the movement of staff between locations reduces the spread of the virus. But will this move stick? It’s difficult to say.
Greater transfer of information has been a significant step forward. The public is now more well-informed both in regards to COVID-19 and pathogens in general. There are official updates everyday, from Ministers of Health in many Canadian jurisdictions and from the Prime Minister. This level of access to information is something that people in historical pandemics did not have, and it has allowed us to react faster.
Whether healthcare’s general preparedness will change in regards to equipment on hand, increased full-time single-site healthcare work, or the general exchange of information is still hard to say at this point. Hopefully things will change for the better. Hopefully steps will be taken. Hopefully.







